Getting a handle on patient education for chronic kidney disease (CKD) is the single most important first step you can take in managing your health. It’s what turns a confusing diagnosis into a clear, actionable plan. With the right knowledge, you can understand your condition, make smart decisions, and become an active partner with your healthcare team in protecting your future.
Understanding Your CKD Diagnosis

Hearing you have chronic kidney disease can feel overwhelming, even a bit isolating. But the most powerful tool you have right now is a clear understanding of what’s happening inside your body.
Think of your kidneys as your body’s silent, highly advanced purification plant. They work around the clock to filter out waste and extra fluid from your blood. A chronic kidney disease diagnosis simply means this plant isn’t running at 100% capacity anymore.
This isn’t a sudden shutdown. It’s a gradual decline in function, often happening so slowly that you might not notice any symptoms until the later stages. This is precisely why proactive patient education is so crucial—it bridges the gap between a medical term and its real-world impact, replacing uncertainty with confidence.
Why Your Kidneys Are So Important
Your two bean-shaped kidneys do much more than just make urine. To truly get a grip on your diagnosis, it helps to appreciate all the vital jobs they perform.
- Waste Filtration: They’re constantly cleaning your blood, removing toxins, urea, and excess salts.
- Fluid Balance: They manage the amount of water in your body to keep you from getting swollen.
- Blood Pressure Control: They release hormones that are key to keeping your blood pressure in check.
- Red Blood Cell Production: They send signals to your body to produce the red blood cells that carry oxygen.
- Bone Health: They activate vitamin D, which your body needs to absorb calcium for strong, healthy bones.
When kidney function starts to dip, all of these connected systems can be affected. This is why managing CKD is about looking at your whole health, not just your kidneys. You can get a deeper dive into this by reading our guide on the signs and steps of a chronic kidney disease diagnosis.
The Most Common Causes in the United States
In the United States, two conditions are behind the vast majority of CKD cases. Understanding these root causes is the key to slowing down any further kidney damage.
The two leading culprits behind chronic kidney disease in the U.S. are diabetes (high blood sugar) and hypertension (high blood pressure). Together, they are responsible for about two-thirds of all cases.
When blood sugar stays consistently high, it acts like sandpaper on the tiny filtering units inside the kidneys, damaging them over time. In a similar way, high blood pressure puts a constant strain on the delicate blood vessels in the kidneys, making them less efficient. This is why a huge part of any CKD management plan involves getting these underlying conditions under control with diet, medication, and lifestyle changes.
Chronic kidney disease is more common than you might think, affecting an estimated 15% of adults in the United States, or about 37 million people. Even more shocking? As many as 9 in 10 adults with CKD have no idea they have it. This statistic from the Centers for Disease Control and Prevention (CDC) highlights the urgent need for better awareness and early education. Taking this journey to educate yourself is the first and most powerful step toward taking back control of your health.
Navigating the Five Stages of Kidney Disease
Chronic kidney disease isn’t something that happens overnight. Instead, it’s a gradual journey that unfolds across several distinct phases. Understanding this progression is a huge part of your education, giving you a clear roadmap of where you are and what’s ahead.
The key number we use to track this journey is your glomerular filtration rate, or GFR. The easiest way to think of your GFR is as a performance score for your kidneys. A higher number means they’re doing a great job filtering your blood, while a lower number shows they’re starting to struggle. This simple number, which comes from a routine blood test, is exactly how doctors determine your CKD stage.
Knowing your stage is incredibly powerful. It helps you and your healthcare team set realistic goals, make smart decisions, and take proactive steps to hang on to the kidney function you still have. You’re no longer just a passive patient; you become an active, knowledgeable partner in your own care.
Stage 1 and Stage 2: The Silent Phase
In Stage 1, your GFR is 90 or higher, which is considered normal or very close to it. The catch is that there might be other subtle signs of kidney damage, like a bit of protein showing up in your urine. Stage 2 is similar, with just a mild drop in function, putting your GFR somewhere between 60 and 89.
Most people in these early stages feel completely fine. There are usually no symptoms, which is exactly why CKD has earned the nickname of a “silent” disease. The name of the game here is prevention.
Your main goals during this phase are to:
- Keep your blood pressure and blood sugar under tight control to prevent more damage.
- Embrace a healthier lifestyle with a balanced diet and regular, gentle exercise.
- Steer clear of medications that can be tough on the kidneys, like certain over-the-counter pain relievers (NSAIDs).
This infographic does a great job of showing how your focus—and your doctor’s—will shift as the disease progresses.
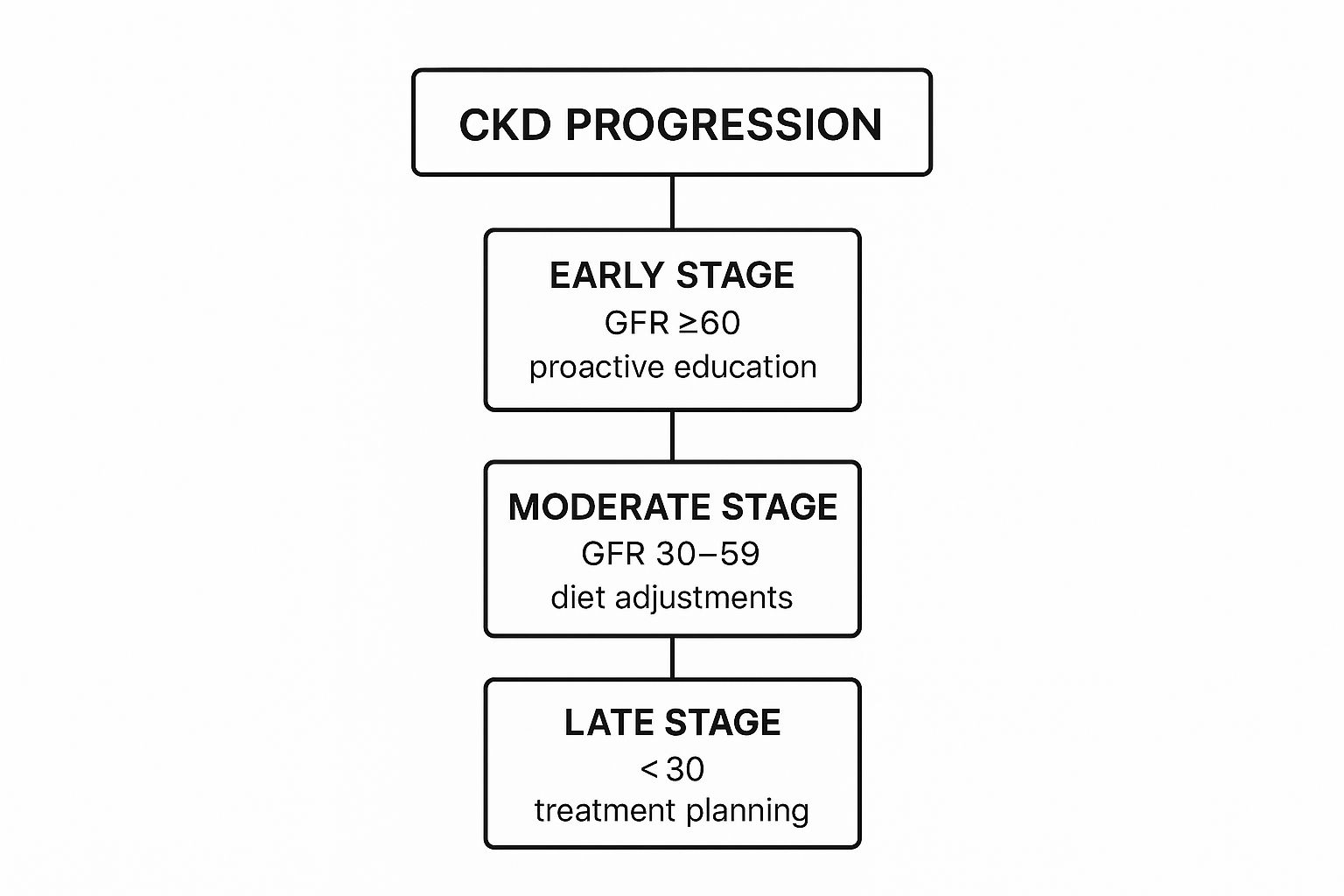
As you can see, it all starts with education in the early stages and moves toward more intensive diet and treatment planning down the line.
Stage 3: The Tipping Point
Stage 3 marks a moderate dip in kidney function, with a GFR between 30 and 59. This is often a major turning point. It’s the stage where symptoms might finally start to creep in, like feeling tired all the time, noticing swelling in your hands and feet, or changes in how often you urinate.
This is usually when your primary care doctor will bring in a nephrologist, a kidney specialist, to join your team. You’ll also start working more closely with them to manage common CKD complications like anemia (low red blood cell count) and bone disease. Diet becomes much more critical now. You can dive deeper into what this stage involves by reviewing detailed information on chronic kidney disease stages.
Stage 4 and Stage 5: Preparing for the Future
When you reach Stage 4, kidney function has severely declined, with a GFR between 15 and 29. Symptoms are often much more noticeable, and the main focus becomes managing complications. This is a critical time for education and getting ready for what might come next.
Your healthcare team will begin discussing your future options, like dialysis or a kidney transplant. These aren’t meant to be scary conversations. They’re designed to give you and your family plenty of time to learn, ask all your questions, and decide on the path that feels right for you.
Stage 5, often called end-stage renal disease (ESRD), is when the GFR drops below 15. At this point, your kidneys simply can’t keep up with your body’s demands on their own. To stay alive and well, you’ll need some form of renal replacement therapy, which means either dialysis or a transplant. The planning that began back in Stage 4 now gets put into motion, making the transition to treatment as smooth as possible.
To help you keep track, here is a quick overview of what each stage means for you.
A Quick Guide to the Five Stages of CKD
| Stage | Description | GFR Level (mL/min) | Recommended Patient Actions |
|---|---|---|---|
| Stage 1 | Normal or near-normal kidney function with some signs of kidney damage. | 90 or higher | Focus on lifestyle: healthy diet, exercise, control blood pressure/sugar. |
| Stage 2 | Mild decrease in kidney function. | 60-89 | Continue with healthy habits and avoid kidney-harming medications (NSAIDs). |
| Stage 3 | Moderate decrease in kidney function. Symptoms may begin to appear. | 30-59 | Work with a nephrologist. Manage complications like anemia and bone disease. |
| Stage 4 | Severe decrease in kidney function. | 15-29 | Actively manage symptoms and begin planning for future treatment options. |
| Stage 5 | End-stage renal disease (ESRD) or kidney failure. | Below 15 | Begin dialysis or proceed with a kidney transplant to sustain life. |
Understanding this path is the first step toward taking control of your health and navigating your CKD journey with confidence.
Your Guide to a Kidney Friendly Diet

When you’re navigating chronic kidney disease, what you put on your plate becomes one of your most powerful tools. Adopting a kidney-friendly diet is a core part of patient education for chronic kidney disease, placing you firmly in control of your health journey.
This isn’t about a bland, restrictive list of foods you can never touch again. Instead, it’s about making smart, deliberate choices that lighten the load on your kidneys. Once you understand why certain nutrients need to be managed, you can create an eating plan that is both sustainable and satisfying.
The main goal is to limit minerals that can build up to unsafe levels in your blood when your kidneys are not filtering at their best. This proactive approach can help you feel better every day and may even slow down the progression of CKD.
Mastering the Key Nutrients Sodium, Potassium, and Phosphorus
Picture your kidneys as incredibly fine-tuned filters. When their function is compromised, certain minerals can slip through and accumulate in your system. The three biggest ones to keep an eye on are sodium, potassium, and phosphorus.
Managing these nutrients is a careful balancing act. Your healthcare team, especially a renal dietitian, will provide you with specific targets based on your lab work and CKD stage. This personalized guidance is what makes your dietary plan truly effective.
Sodium’s Role in Fluid and Blood Pressure
Sodium, which we mostly get from salt, acts like a sponge for water. Too much sodium causes your body to retain extra fluid. This can lead to swelling, shortness of breath, and, most importantly, high blood pressure.
Since high blood pressure is a primary driver of kidney damage, getting your sodium intake under control is absolutely essential. The average American consumes over 3,400 milligrams of sodium daily, but people with kidney disease often need to aim for less than 2,300 milligrams—sometimes even lower, as recommended by the American Heart Association.
The most impactful first step is cutting back on processed, packaged, and restaurant foods. These are the biggest culprits for hidden sodium. Cooking more meals at home with fresh ingredients and salt-free seasonings gives you total command over your intake.
Learning to read the Nutrition Facts label on food packaging is another vital skill. Look for keywords like “low sodium” or “sodium-free.” You can also compare the sodium content per serving on different brands to make a healthier choice.
Potassium and Phosphorus The Hidden Minerals
Potassium is crucial for your nerves and muscles, but when levels get too high, it can be dangerous for your heart. Phosphorus is key for strong bones, but an excess amount can leach calcium from your bones, making them brittle, and can also lead to intensely itchy skin.
These two minerals can be tricky because they show up in many foods we think of as healthy.
- High-Potassium Foods to Limit: Think bananas, oranges, potatoes, tomatoes, and most dairy products.
- High-Phosphorus Foods to Watch: This includes dairy, nuts, beans, and especially dark-colored sodas, which often have phosphorus additives.
Don’t worry, your dietitian can show you plenty of delicious lower-potassium and lower-phosphorus swaps so you never feel like you’re missing out.
The Protein Puzzle How Much is Right for You
Protein is vital for building muscle and repairing tissue, but it’s another nutrient that needs careful management with CKD. When your body breaks down protein, it produces a waste product called urea. Healthy kidneys have no problem filtering urea out, but with CKD, it can build up in the blood and make you feel tired and unwell.
The right amount of protein is highly individual. In the earlier stages of CKD, your doctor might recommend a lower-protein diet to reduce the strain on your kidneys. If you eventually progress to dialysis, however, your protein needs will actually go up because the dialysis process removes some protein from your body.
This is precisely why working with a renal dietitian is so important. They will help you find that “just right” protein balance for your specific stage, making sure you get enough to stay strong without overwhelming your kidneys. They will guide you toward high-quality sources like lean meats, fish, and eggs in the right portion sizes, ensuring your diet is safe, effective, and tailored perfectly to you.
Making Lifestyle Changes That Protect Your Kidneys
While a kidney-friendly diet is a cornerstone of managing CKD, what you do every day matters just as much. Making thoughtful lifestyle changes is a critical part of your patient education for chronic kidney disease, as your daily habits directly impact the very conditions that often cause kidney damage in the first place.
Think of these changes not as a list of restrictions, but as powerful acts of self-care. Every positive choice you make—from managing your blood pressure to simply moving your body more—helps lighten the incredible workload your kidneys handle, preserving their function for the long haul. This is your chance to step up and become an active, empowered partner in your own health journey.
Keeping Blood Pressure and Blood Sugar in Check
High blood pressure and high blood sugar are, without a doubt, the two biggest threats to your kidney health. When these numbers stay elevated over time, they slowly but surely damage the tiny, delicate blood vessels inside your kidneys, making it much harder for them to filter your blood effectively.
Bringing these numbers down into a healthy range is arguably the single most important thing you can do to slow down CKD. This means working with your doctor to take medications as prescribed, monitoring your levels at home, and fully committing to the diet and exercise habits that keep those numbers stable.
Finding Physical Activities You Enjoy
Regular physical activity is a game-changer. It helps control blood pressure and blood sugar, boosts your mood, and fights fatigue. The real secret, though, is finding activities you actually enjoy. That’s how movement becomes a sustainable part of your life, not just another chore on your to-do list.
You don’t need to run a marathon. Consistency is what counts, not intensity.
- Start Small: Begin with short, gentle walks. As you get stronger, you can gradually increase your time and distance.
- Explore Options: Try low-impact activities that are easier on your joints, like swimming, cycling, or yoga.
- Listen to Your Body: It’s totally normal to feel tired, especially if you’re also managing anemia. Rest when you need to, and celebrate the small victories along the way.
Always have a conversation with your doctor before starting a new exercise program. They can help you create a plan that’s both safe and effective for your specific stage of CKD and overall health.
Managing a chronic condition like CKD isn’t just about physical health; it’s also about emotional well-being. Chronic stress can raise your blood pressure and blood sugar, creating a vicious cycle that can further harm your kidneys. Finding healthy ways to cope is absolutely essential.
The Critical Decision to Quit Smoking
If you smoke, quitting is one of the best decisions you can possibly make for your kidneys and your heart. Smoking wreaks havoc on blood vessels throughout your body, which reduces blood flow to your kidneys and speeds up the progression of CKD.
The good news is that the benefits start almost immediately. Your blood pressure begins to drop and your circulation improves, giving your kidneys a much-needed break. Don’t go it alone—ask your healthcare team for resources. In the U.S., you can call 1-800-QUIT-NOW for free support.
CKD is a massive global health issue, affecting an estimated 10% of the world’s population, with major gaps in access to care. The Global Burden of Disease study showed that CKD jumped from the 27th leading cause of death in 1990 to the 18th in 2010, which underscores the urgent need for better education and proactive management. You can read more about the global impact of CKD to understand the scale of this challenge.
Building Your Emotional Support System
Living with a chronic illness can be emotionally draining. It’s perfectly normal to feel overwhelmed, anxious, or down from time to time. That’s why building a strong support system is so crucial for navigating these feelings.
Your network might include family, close friends, a therapist, or even a support group with other people who understand exactly what you’re going through. The National Kidney Foundation (NKF) offers peer support programs and local resources across the United States. Sharing your experiences can make you feel less isolated and give you practical strategies for coping. Taking care of your mental health isn’t an extra—it’s a vital part of a truly complete care plan.
Getting to Know Your Medications and Treatments
When you’re dealing with chronic kidney disease, a new list of medications can feel a little overwhelming. But think of each prescription as a key player on your personal health team, each one with a specific job to do. Understanding why you’re taking each one is a huge part of your care—it empowers you to stay on track and be an active partner in your own health.
Your medications are like a dedicated support crew. One might be in charge of keeping your blood pressure in a healthy range, while another is tasked with managing fluid levels. They all work together to protect your remaining kidney function and help you feel as good as possible.
Common Medications to Protect Your Kidneys
Your doctor will hand-pick medications based on your specific needs, your CKD stage, and other health conditions like diabetes or heart disease. While your regimen is unique to you, there are a few common types of medications that are superstars in kidney care in the U.S.
- ACE Inhibitors and ARBs: These are the front-line defenders for your kidneys. They work by relaxing your blood vessels, which brings down your blood pressure and eases the strain on your kidneys’ delicate filtering system.
- Diuretics (Water Pills): If your kidneys aren’t removing enough fluid on their own, diuretics give them a helping hand. They help your body flush out extra salt and water, which can reduce swelling and lower blood pressure.
- Phosphate Binders: You’ll take these with meals. They act like little magnets, grabbing onto excess phosphorus from your food so it doesn’t build up to unsafe levels in your blood.
- Anemia Treatments: CKD can mess with your body’s ability to produce red blood cells, leaving you feeling tired and worn out. Your doctor might prescribe iron supplements or injections of erythropoietin-stimulating agents (ESAs) to kickstart red blood cell production.
The best thing you can do is have open, honest conversations with your healthcare team about your medications. When you understand the “why” behind each pill and its potential side effects, you’re no longer just a patient—you’re the CEO of your health.
When Your Kidneys Need a Little More Help
As kidney function declines into the later stages, there will come a time when your body needs more support than medications alone can provide. This is when your care team will start talking about renal replacement therapy. This isn’t a setback; it’s just the next proactive step on your health journey.
The two main paths forward are dialysis and kidney transplantation. The goal is to work with your team to figure out which option best aligns with your health, your lifestyle, and what feels right for you.
Looking at Your Dialysis Options
Dialysis is a life-saving treatment that steps in to do the job your kidneys can no longer manage, filtering out waste and extra fluid from your blood. There are two main ways it’s done, each with a different approach.
- Hemodialysis (HD): This is the most common type. Your blood is filtered by a machine outside your body. Most people go to a dialysis center for this, typically three times a week for a few hours at a time, but some folks are trained to do it right at home.
- Peritoneal Dialysis (PD): This clever method uses the lining of your own belly (the peritoneum) as a natural filter. A special cleansing fluid goes in through a catheter, pulls out waste products, and is then drained away. The big plus here is flexibility—you can often do it at home, even while you sleep.
The Journey to a Kidney Transplant
For many, a kidney transplant represents a chance for a life with fewer restrictions than dialysis allows. It’s a surgery where a healthy kidney from a deceased or a living donor is placed in your body.
Getting to a transplant involves a very thorough evaluation to make sure it’s a safe and viable option for you. In the United States, patients are placed on a national waiting list managed by the United Network for Organ Sharing (UNOS). While it does mean a lifelong commitment to taking anti-rejection medications, a successful transplant can be a game-changer, restoring kidney function and dramatically improving your quality of life. Making these big decisions takes time, education, and plenty of heartfelt talks with your family and your medical team.
How to Be an Active Partner in Your CKD Care
When it comes to your health, you’re the most important person on the team. While your doctors and nurses provide essential guidance, it’s your day-to-day actions and observations that truly steer the course of your CKD journey. Taking charge and becoming a confident advocate is one of the most powerful things you can do—it shifts you from simply receiving care to actively participating in it.
This change in perspective is huge. It helps ensure your treatment plan doesn’t just check medical boxes but also fits your life, your goals, and what matters most to you. It all begins with a few straightforward, effective strategies you can start using right away.
Monitoring Your Health at Home
Your health journey isn’t just happening in the doctor’s office; it’s unfolding every single day at home. Simple at-home monitoring gives you and your care team a real-time picture of how your body is doing, providing valuable information that helps guide the best decisions.
One of the most impactful habits you can build is tracking your blood pressure. High blood pressure is a primary driver of kidney damage, so keeping a daily log can reveal patterns that a single reading at the clinic would completely miss.
Similarly, keeping an eye on your weight helps you and your doctor manage fluid balance, which is often a challenge with CKD. A sudden jump on the scale over just a day or two can be an early warning sign that your body is retaining too much fluid.
Making the Most of Your Doctor Visits
Your time with the doctor is precious, and a little bit of prep work goes a long way. Instead of just showing up, take a few moments before your appointment to think about what you need to get out of it.
Come to every appointment with a written list of your top three questions or concerns. This simple step ensures you address what’s most important to you and don’t forget anything in the moment.
Before you head out the door, try to:
- Review Your Numbers: Bring your home blood pressure and weight logs.
- Update Your Medication List: Make a note of any changes, including over-the-counter medicines or supplements you’ve started.
- Jot Down Symptoms: Write down anything new or different you’ve been feeling, no matter how minor it seems.
This kind of preparation turns your appointment from a monologue into a productive, two-way conversation. Unfortunately, not all educational materials are created to help you do this. One study revealed that nearly half of all CKD patient handouts were written at a high reading level, and a mere 20% were considered superior quality. You can learn more about the quality gap in patient education and see why being your own advocate is so critical.
Clear communication is your superpower here. Never hesitate to say, “Can you explain that in a simpler way?” or “What do these lab results actually mean for me?” When you state your needs clearly and ask direct questions, you step into a role of shared decision-making, helping to create a care plan that genuinely works for you.
Common Questions About Living with CKD
Living with a long-term condition like CKD will naturally bring up a lot of questions. Getting clear, straightforward answers is a huge part of feeling confident and in control of your health.
Below, we’ll tackle some of the most common questions we hear from people who are navigating their own CKD journey.
Can Chronic Kidney Disease Be Reversed?
This is often the very first question people ask, and the honest answer is that CKD is a progressive condition that can’t be truly reversed. However—and this is a big however—its progression can often be slowed down significantly. The best way to think about it is less like curing a cold and more like carefully managing a delicate garden.
Early diagnosis is absolutely key. When you catch it early and diligently manage the root causes, like high blood pressure or diabetes, you can make a massive difference. By sticking to a kidney-friendly diet, taking your medications as prescribed, and making healthier lifestyle choices, you are actively preserving your remaining kidney function for as long as possible.
The goal of CKD management is preservation, not reversal. Every positive step you take is a powerful investment in slowing down damage and protecting your quality of life.
What Are the First Signs of Chronic Kidney Disease?
In the early stages, CKD is often called a “silent” disease for a good reason—it usually has no symptoms you can see or feel. This is exactly why regular check-ups with your doctor are so important, especially if you have any risk factors like diabetes or a family history of kidney issues.
As the condition progresses, you might start to notice subtle signs that something is off. These can include:
- Feeling unusually tired or persistent fatigue
- Swelling (edema) in your legs, ankles, or feet
- Needing to urinate more often, especially at night
- Seeing foam or bubbles in your urine
Because these symptoms are so vague and can be linked to many other things, routine blood and urine tests are the only reliable way to catch CKD early.
How Often Should I See My Doctor If I Have CKD?
How often you’ll need to see your doctor really depends on your specific CKD stage and your overall health. If you’re in the early stages, you might just see your primary care provider every six to 12 months for monitoring.
As the disease moves into later stages, it’s very likely you’ll be referred to a nephrologist, who is a kidney specialist. At that point, your visits will probably become more frequent—maybe every one to three months. Your healthcare team will work with you to create a personalized follow-up schedule based on your lab results and how well your condition is being managed.
At Medilux Ayurveda USA, we believe that knowledge is power. We’re here to provide you with holistic support for your kidney health journey. Our authentic, herb-based treatments and personalized care plans are designed to help improve kidney function and your overall well-being. To learn more, explore our programs at Medilux Ayurveda.
