A diet for chronic kidney disease (CKD) isn’t about harsh restrictions. Think of it as a strategic plan designed to protect your kidneys and, just as importantly, improve your quality of life. The main goal is to carefully manage nutrients like sodium, potassium, phosphorus, and protein. By doing this, you lighten the filtering load on your kidneys, which can help slow the disease’s progression and keep symptoms in check.
Why Your Diet Is Crucial for Kidney Health
Imagine your kidneys as a highly sophisticated filtering system for your body. Day after day, they work around the clock, removing waste and extra fluid from your blood to keep everything in perfect balance. When chronic kidney disease sets in, this filtering power starts to decline.
This means that waste products, which should be flushed out, can begin to accumulate in your bloodstream. Over time, this buildup can cause serious health issues, including high blood pressure, fluid retention (edema), bone disease, and heart problems. This is where a specialized diet for chronic kidney disease becomes your most powerful tool.
Easing the Burden on Your Kidneys
The core idea of a renal diet is simple: reduce the workload on your kidneys. By keeping a close eye on certain minerals and nutrients, you can stop them from reaching dangerous levels in your body. It’s a proactive way to take charge of your health and hold onto your remaining kidney function for as long as possible.
The key players in this dietary strategy usually involve:
- Managing Sodium: Cutting back on sodium is a game-changer for controlling blood pressure and reducing fluid buildup. Both of these put extra strain on your kidneys and heart.
- Controlling Potassium: When kidneys are damaged, they can’t remove excess potassium very well. High levels can lead to dangerous heart rhythm problems, so keeping it in check is vital.
- Limiting Phosphorus: Too much phosphorus in your blood can pull calcium from your bones, making them weak and brittle. It can also cause harmful calcium deposits in your blood vessels.
- Adjusting Protein: Protein is essential, but your body creates waste when it breaks it down. Adjusting how much you eat reduces the amount of waste your kidneys have to filter.
A well-managed renal diet is far more than a list of rules; it’s a way for you to actively participate in your own care. The food choices you make every day can directly impact your symptoms, slow down CKD, and help you maintain a better quality of life.
Your Path Is Unique
It’s critical to understand that there is no one-size-fits-all diet for chronic kidney disease. Your specific dietary needs will shift depending on your stage of CKD, your latest lab results, and your overall health. For example, someone in the early stages might only need to watch their sodium intake. In contrast, a person in a later stage will likely have much stricter limits on potassium, phosphorus, and even fluid.
This is exactly why working with a professional is non-negotiable. A U.S.-based healthcare provider or a registered renal dietitian is absolutely essential for creating a personalized plan that is both safe and effective for you. They can help you make sense of all these complexities, ensuring your diet works for you. For more information on navigating your condition, explore our guide on patient education for chronic kidney disease.
Understanding the Four Pillars of a Renal Diet
Adopting a diet for chronic kidney disease can feel like learning an entirely new language. To truly get it right, it helps to understand the “why” behind every recommendation. Think of the renal diet as a strong structure supported by four essential pillars: managing protein, sodium, phosphorus, and potassium. Each one plays a unique and powerful role in protecting your remaining kidney function.
Once you grasp how these nutrients impact your body, making informed and confident food choices becomes second nature. Let’s break down their roles with some simple analogies to make these concepts stick.
Protein: The Delicate Balance of Building and Cleaning
Protein is absolutely essential for building muscle and repairing tissue, but it’s a bit of a double-edged sword for those with CKD. Imagine protein is the fuel that powers your body. Like any fuel, it leaves behind a byproduct after it’s burned—in this case, waste products like urea.
Healthy kidneys are like an efficient cleaning crew, easily filtering this “ash” out of your blood. But when kidney function is compromised, that crew is understaffed. The waste builds up, creating a toxic environment that can leave you feeling tired and sick. The goal isn’t to eliminate protein but to manage your intake, providing just enough fuel without overwhelming the cleaning crew.
This infographic simplifies how the key components of a renal diet work together to support your kidneys.
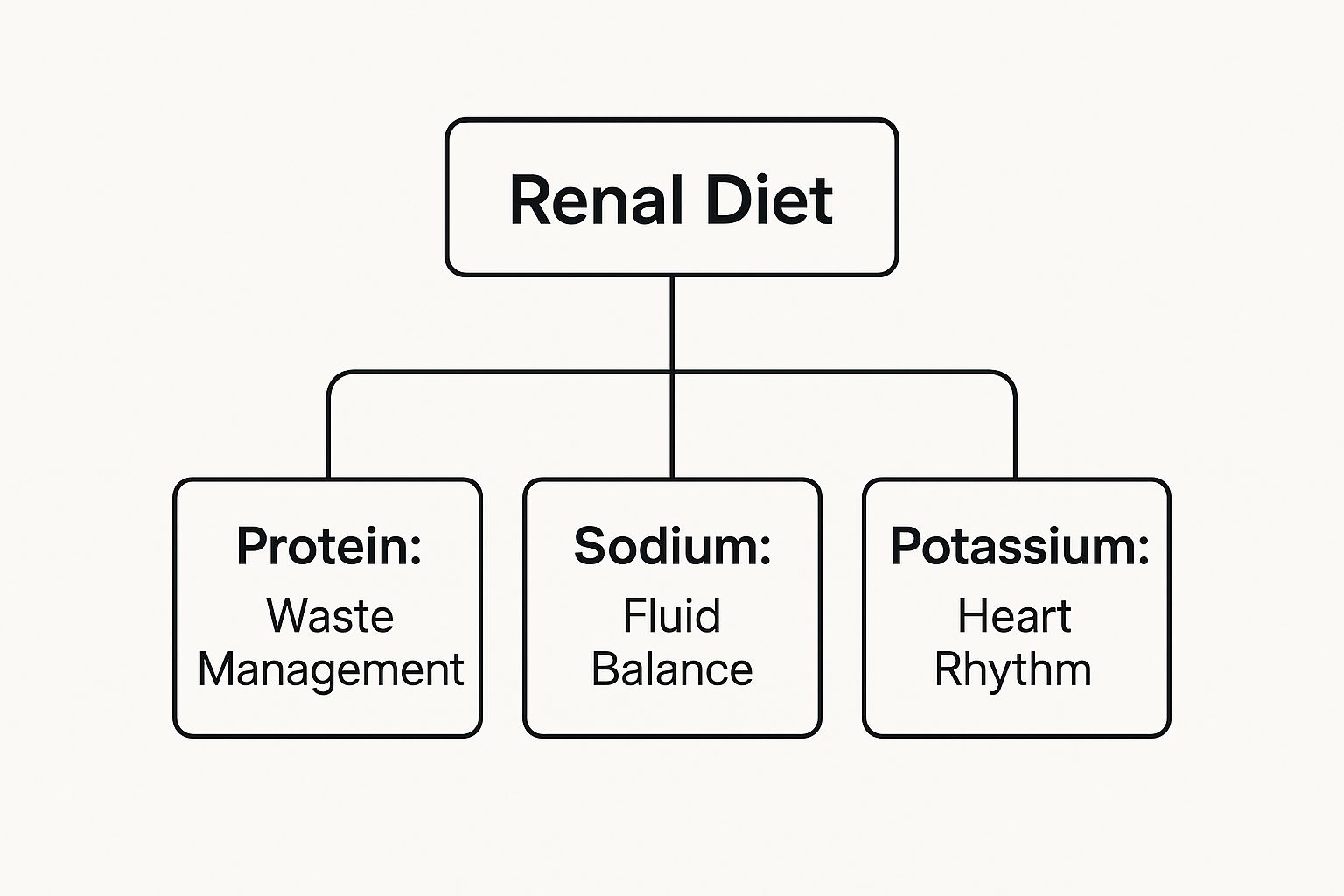
As the diagram shows, managing protein, sodium, and potassium are distinct but interconnected strategies for maintaining your overall health with CKD.
Sodium: The Magnet for Fluid
Think of sodium as a magnet for water. When you eat too much salt, your body holds onto extra fluid to dilute it, much like you’d add water to an overly salty soup. This excess fluid increases the volume of blood circulating through your vessels.
This forces your heart to pump harder and raises your blood pressure, putting immense strain on both your cardiovascular system and your already-strained kidneys. High blood pressure is a leading cause of kidney damage, so controlling sodium is one of the most impactful changes you can make. By cutting back, you help lower blood pressure, reduce swelling (edema), and ease the workload on your heart and kidneys.
Managing sodium intake is foundational to any diet for chronic kidney disease. It directly influences blood pressure and fluid retention, two critical factors in preserving remaining kidney function and preventing complications.
This principle goes way beyond just avoiding the salt shaker. Processed foods, canned soups, and restaurant meals are often packed with hidden sodium. Globally, chronic kidney disease linked to dietary risk factors has shown a marked increase in both mortality and disability rates over recent decades. The most significant dietary risk is actually the consumption of sugar-sweetened beverages. You can explore the full study on dietary risks and kidney disease to learn more about how global dietary trends impact CKD.
Phosphorus and Potassium: The Mineral Regulators
In a healthy body, the kidneys act as master regulators, keeping minerals like phosphorus and potassium in perfect balance. When their function declines, this delicate equilibrium is disrupted, and levels of these minerals can rise to dangerous heights.
- Phosphorus: When phosphorus builds up, it can pull calcium right out of your bones, leaving them weak and brittle. This rogue calcium can then deposit in your blood vessels, heart, and skin, causing serious cardiovascular problems.
- Potassium: This mineral is vital for nerve function and keeping your heart beating steadily. However, too much potassium (a condition called hyperkalemia) can lead to life-threatening irregular heart rhythms.
By being mindful of high-phosphorus foods (like dairy, processed meats, and dark colas) and high-potassium foods (like potatoes, tomatoes, and bananas), you help prevent these serious complications. It’s all about carefully selecting foods to maintain that crucial mineral balance your kidneys can no longer manage on their own.
Building Your Kidney-Friendly Plate
Knowing the theory behind protein, sodium, phosphorus, and potassium is the first step. Now, it’s time to put that knowledge into practice—translating it into real-world choices you can make at the grocery store or when you open your fridge. Crafting a diet for chronic kidney disease is really about making smart swaps and knowing exactly what to look for in each food group.
This section will break down how to approach the major food categories, giving you the confidence to build meals that protect your kidneys without making you feel like you’re missing out. We’ll focus on practical, simple swaps and how to read labels like a pro, putting you back in control of what’s on your plate.

Prioritizing High-Quality Protein
Protein is a cornerstone of any renal diet, but it’s a bit of a balancing act. The key is to focus on high-quality protein sources in portions that your dietitian has recommended for you. Think of these proteins as being more efficient; they give your body all the essential building blocks it needs while creating less metabolic waste for your already-strained kidneys to filter.
Poor dietary choices can have a staggering impact on kidney health. In fact, data from 2021 showed that dietary risks were behind roughly 20.8% of all global CKD-related deaths. A major contributor was high consumption of red and processed meats, which shows just how critical mindful protein selection is. You can learn more about these findings on dietary risks and kidney disease to understand the bigger picture.
- Choose This: Go for lean proteins like skinless chicken or turkey breast, fish (especially those rich in omega-3s like salmon), and egg whites. These are all excellent choices that are much easier on your kidneys.
- Limit This: It’s best to cut back on processed meats like bacon, sausage, and deli meats, as they are often packed with sodium and phosphorus additives. Red meat should also be eaten in moderation because it creates a higher load of waste products.
Navigating Fruits and Vegetables
Fruits and vegetables are full of vitamins and antioxidants, but for someone with CKD, they also present a potassium challenge. The goal isn’t to avoid them entirely but to choose wisely. This is where a renal dietitian is invaluable in helping you understand your personal potassium limits.
The “Choose This” vs. “Limit This” approach is about empowerment, not deprivation. By learning which foods are lower in potassium and phosphorus, you can still enjoy a colorful and varied diet that supports your kidney health.
For instance, you can absolutely enjoy a delicious fruit salad or a side of steamed vegetables with dinner. It’s all about selecting the right ingredients to begin with.
A great way to visualize this is to compare common choices side-by-side.
Low vs High Potassium Foods for a Kidney Diet
This table breaks down some common fruits and vegetables, categorizing them based on their typical potassium content. Use it as a handy guide when planning your meals.
| Lower-Potassium Choices (Generally <200mg per serving) | Higher-Potassium Choices (Limit or Avoid, >200mg per serving) |
|---|---|
| Apples | Bananas |
| Berries (strawberries, blueberries) | Oranges & Orange Juice |
| Grapes | Potatoes & Sweet Potatoes |
| Pineapple | Tomatoes & Tomato Sauce |
| Cauliflower | Avocados |
| Cabbage | Spinach (cooked) |
| Cucumbers | Winter Squash (acorn, butternut) |
| Bell Peppers (especially green) | Artichokes |
Remember, portion size is key. Even lower-potassium foods can add up if eaten in large quantities, so always be mindful of how much you’re eating in one sitting.
Making Smart Grain Selections
Grains are a staple for many of us, but the type of grain you choose matters a great deal on a kidney diet. While whole grains are often touted for their health benefits, they are also typically higher in phosphorus and potassium. For this reason, refined grains are often the safer bet.
- Choose This: White bread, sourdough, white rice, and pasta made from refined flour are lower in phosphorus and are generally better choices.
- Limit This: Whole wheat bread, brown rice, bran cereals, and oatmeal contain more phosphorus and may need to be restricted based on your lab results.
Dairy and Dairy Alternatives
Dairy products are a fantastic source of calcium, but they are also very high in phosphorus and potassium. This makes managing dairy a critical part of your plan. Fortunately, there are many alternatives on the market that can fit more easily into a renal diet.
When picking a dairy alternative like almond or rice milk, always be sure to check the label. Some brands are fortified with calcium phosphate, which is an additive you want to avoid.
- Choose This: Look for unenriched rice milk, almond milk, or soy milk. Small amounts of certain dairy like cottage cheese or Greek yogurt might be okay, but you must check with your dietitian first.
- Limit This: Milk, hard cheeses, and processed cheese products are usually very high in both phosphorus and sodium.
Finally, your superpower in all of this is becoming an expert at reading food labels. Manufacturers often add phosphorus- and sodium-based additives to processed foods for flavor and preservation. Learning to spot words containing “phos” in the ingredients list is an essential skill. For a helpful guide, check out our low-sodium foods chart to make your next grocery trip easier.
Exploring Plant-Forward Eating for CKD
Recent research is shedding light on a powerful strategy for managing chronic kidney disease: making a simple shift toward more plant-based foods. This isn’t about becoming a strict vegetarian or vegan overnight. Instead, think of it as a flexible approach, often called “plant-forward” eating, that puts vegetables, legumes, and whole grains at the center of your plate.
For anyone navigating a diet for chronic kidney disease, this change can be a game-changer. Plant-based proteins are often much gentler on the kidneys than many animal proteins, creating less metabolic waste for your body to filter. This one adjustment can significantly ease the workload on your entire system.

The Phosphorus Advantage of Plants
One of the biggest wins of plant-forward eating comes down to phosphorus management. While plenty of plant foods like beans and nuts do contain phosphorus, it’s a specific type called phytate-bound phosphorus. The key difference? Your body finds it much harder to absorb this form, which means less of it ever makes it into your bloodstream.
On the flip side, the phosphorus in animal proteins is much more readily absorbed. Even worse are the phosphorus additives lurking in processed foods, which are nearly 100% absorbed by the body. By simply choosing more whole plant foods, you naturally lower your phosphorus load.
Think of it this way: plant-based phosphorus is like a key that doesn’t quite fit the lock of your digestive system. Much of it just passes right through without being absorbed, making it a far safer choice for protecting your bones and heart.
Broader Benefits for Kidney Health
Beyond just phosphorus control, a plant-forward diet lines up perfectly with the broader goals of CKD management. Many people who start incorporating more plants into their meals notice positive shifts in some of their most important health markers.
These benefits often include:
- Lower Acid Load: Animal proteins generate more acid when your body metabolizes them, and it’s the kidneys’ job to neutralize it. A diet full of fruits and vegetables creates a much lower acid load, taking a lot of that pressure off.
- Better Blood Pressure: Plant-based diets are naturally lower in sodium and higher in fiber, two factors that contribute to better blood pressure control—a critical piece of the puzzle for slowing CKD progression.
- Reduced Inflammation: So many plant foods are bursting with antioxidants and anti-inflammatory compounds. These can help combat the chronic inflammation that often goes hand-in-hand with kidney disease.
Of course, the quality of your plant-based diet really matters. A 2023 study highlighted by the National Kidney Foundation found that a healthy diet rich in whole grains, fruits, and vegetables was linked to a lower risk of mortality for people with CKD. In contrast, an unhealthy plant-based diet full of refined foods and sugars led to worse outcomes.
Simple Ways to Get Started
You don’t have to overhaul your entire life to start eating more plant-forward. The best approach is gradual, making small, sustainable changes that feel right for you. If you’re curious about which specific vegetables to start with, our guide on what vegetables are good for the kidneys is a great resource.
Here are a few easy ideas to get you going:
- Embrace Meatless Mondays: Pick one day a week to go completely vegetarian. It’s a fantastic, low-pressure way to explore new recipes and flavors.
- Make Smart Swaps: Try replacing half the ground meat in a recipe like chili or bolognese with lentils or mashed beans. You’ll boost the fiber and cut back on animal protein without losing that hearty texture.
- Rethink Your Plate: Instead of having meat as the main event, treat it like a side dish. Fill the majority of your plate with vibrant vegetables, salads, and kidney-friendly grains.
A Sample 3-Day Kidney-Friendly Meal Plan
Theory is one thing, but actually seeing how the principles of a diet for chronic kidney disease come together on a plate makes all the difference. To help you visualize what this looks like, we’ve put together a sample 3-day meal plan.
Think of this less as a strict prescription and more as a template. It’s here to show you how balanced, flavorful, and satisfying kidney-friendly eating can truly be. This plan focuses on whole foods, smart portions, and simple cooking methods to keep sodium, potassium, and phosphorus in check. Of course, this is just a starting point—your registered dietitian can help you customize it based on your specific lab results and personal tastes.

Day 1: A Gentle Introduction
Kicking off your day with a kidney-friendly breakfast sets a positive tone. This first day focuses on simple, easy-to-prepare meals that are naturally low in the minerals you need to monitor.
- Breakfast: ½ cup of cooked cream of rice with a sprinkle of cinnamon and 1 teaspoon of honey, paired with ½ cup of fresh blueberries.
- Lunch: A turkey sandwich made with 2 ounces of low-sodium, roasted turkey breast on two slices of sourdough bread, with lettuce and sliced cucumber.
- Dinner: 3 ounces of baked salmon seasoned with lemon and dill, served with 1 cup of white rice and ½ cup of steamed green beans.
Day 2: Flavorful and Familiar Favorites
Day two is all about showing you how to adapt familiar meals to fit your renal diet. With just a few simple swaps, you can still enjoy classic comfort foods without the worry. You’ll notice how herbs and spices easily step in to replace salt for flavor.
- Breakfast: Two scrambled egg whites with chopped bell peppers and onions, served with one slice of white toast and a small amount of unsalted butter.
- Lunch: A vibrant salad with 2 cups of mixed greens, grilled chicken strips (2 ounces), sliced radishes, and cucumbers. Top it with a simple vinaigrette made from olive oil and red wine vinegar.
- Dinner: Homemade chicken stir-fry with 3 ounces of chicken, ½ cup of broccoli florets, and sliced carrots, cooked with low-sodium soy sauce, garlic, and ginger. Serve over 1 cup of cooked white rice.
Key Takeaway: Planning is your best tool. By preparing meals at home, you have complete control over every ingredient. This ensures your dishes are low in sodium and free from hidden phosphorus additives often found in restaurant or processed foods.
Day 3: Keeping It Simple and Satisfying
The final day emphasizes meals that are both easy to assemble and delicious. It’s proof that a diet for chronic kidney disease doesn’t have to be complicated or time-consuming.
- Breakfast: ½ cup of cooked oatmeal (made from quick-cooking oats, not whole-rolled oats) topped with ½ cup of sliced peaches (canned in juice, drained).
- Lunch: A small bowl of low-sodium chicken noodle soup (using homemade or specially marked low-sodium broth) with a side of unsalted crackers.
- Dinner: 3 ounces of lean ground turkey meatballs (made without breadcrumbs or with low-phosphorus bread) simmered in a low-potassium tomato sauce, served over 1 cup of regular pasta.
These examples are designed to spark some inspiration and prove that a kidney-friendly diet can be varied and genuinely enjoyable.
To give you a clearer picture, the table below provides a rough estimate of the daily nutrient totals for this plan. It helps show how these meals align with typical CKD goals.
Nutrient Estimates for Sample Meal Plan (Per Day)
This table provides an approximate daily breakdown of key nutrients for the sample meal plan, demonstrating how the meals align with typical CKD dietary goals.
| Day | Sodium (mg) | Potassium (mg) | Phosphorus (mg) | Protein (g) |
|---|---|---|---|---|
| 1 | ~1,200 | ~1,800 | ~750 | ~60 |
| 2 | ~1,400 | ~2,000 | ~800 | ~65 |
| 3 | ~1,300 | ~1,900 | ~780 | ~62 |
As you can see, a little planning goes a long way in managing your nutrient intake while still enjoying a satisfying menu.
Making Your Renal Diet a Sustainable Lifestyle
Long-term success with a diet for chronic kidney disease isn’t about being perfect. It’s about making it a natural part of your life. The real goal is to weave this new way of eating into your daily routine so it feels normal, not like a chore. Thriving with a renal diet means finding joy in your food again, just with a bit more mindfulness.
This shift begins right in your kitchen but doesn’t stop there. It extends to family dinners, holidays, and nights out. The key is to see this diet not as a set of rules holding you back, but as a powerful tool you can use every single day to take control of your health.
Master Your Kitchen with Flavor
When you have to cut back on salt, flavor becomes your new best friend. Instead of reaching for the salt shaker, this is your chance to explore the incredible world of herbs and spices. It’s an opportunity to get creative and find new taste combinations that you absolutely love.
Think of it as building a whole new flavor toolkit.
- Bright & Zesty: A squeeze of lemon juice, some lime zest, or a splash of vinegar can add a bright, tangy kick that your taste buds will appreciate.
- Aromatic & Earthy: Things like garlic powder (not garlic salt!), onion powder, smoked paprika, and cumin can create those deep, savory flavors we all crave.
- Fresh & Herbaceous: Fresh herbs are a game-changer. Cilantro, parsley, dill, and rosemary can add a burst of freshness that brings simple meals to life.
By playing around with these, you’ll quickly find that low-sodium food can be incredibly delicious, proving that kidney-friendly eating is anything but bland.
Navigating Social Situations and Dining Out
Going out to eat or attending a party can feel a little intimidating at first, but with a bit of planning, you can handle it like a pro. The most important thing is to not be afraid to speak up for your needs.
When you’re dining out, check the menu online beforehand or call the restaurant. Most chefs are more than willing to accommodate requests like leaving the salt out of a dish. Simple preparations like grilled fish or chicken with steamed veggies are often a safe and tasty bet.
The most important partnership you can build is with a registered renal dietitian. They are your single best resource for personalizing your plan, answering your unique questions, and helping you navigate the complexities of a CKD diet for long-term success.
Hydration and Your Personal Plan
Finally, let’s talk about hydration. This is a critical piece of the puzzle, but it’s also highly individual. Someone in the early stages of CKD might not have any fluid restrictions, while those in later stages often need to watch their intake very carefully. If it’s necessary, your doctor will give you a specific daily fluid limit.
Sticking to that recommendation is absolutely essential for managing your blood pressure, preventing swelling, and reducing the strain on your heart. It’s just one more way you can take an active role in living a healthier, fuller life with CKD.
Your Top Questions About the CKD Diet, Answered
Starting a new way of eating always brings up a few questions. When you’re managing a diet for chronic kidney disease, it’s only natural to wonder about specific foods, day-to-day challenges, and how to build lasting habits. This section tackles some of the most common points of confusion head-on.
My goal here is to give you the confidence to handle everyday food situations with ease. Once you have the right information, you can make smart, kidney-friendly choices that truly support your health and well-being.
Do I Have to Give Up All My Favorite Foods?
Absolutely not! A kidney diet that you can stick with for the long haul is built on moderation and smart substitutions, not total deprivation. You’d be surprised how many of your favorite recipes can be tweaked to fit your new guidelines.
For instance, that pasta dish you love can be made kidney-friendly by swapping in a low-potassium tomato sauce, keeping an eye on the protein portion, and leaving out high-sodium processed meats. A renal dietitian is a pro at helping you find these clever swaps so you can still enjoy the foods that bring you joy.
Can I Use Salt Substitutes?
This is one area where you need to be extremely cautious. Most salt substitutes get their salty flavor by replacing sodium chloride with potassium chloride. For anyone with compromised kidneys, this can be a dangerous trade.
When kidneys aren’t working at full capacity, they struggle to filter excess potassium from the blood. Using these substitutes can cause your potassium levels to climb to unsafe heights—a condition called hyperkalemia that can seriously impact your heart rhythm.
The best and most flavorful path is to become friends with your spice rack. Get creative with garlic powder, onion powder, smoked paprika, dill, oregano, and even a fresh squeeze of lemon juice to bring your dishes to life without the risk.
How Important Is Fluid Intake on a CKD Diet?
Managing your fluids is a very personal part of the diet for chronic kidney disease. Your exact needs will depend entirely on your stage of CKD and what your lab results show. In the early stages, you might not have any fluid restrictions at all.
As kidney function declines, however, your body can lose its ability to get rid of extra water. This can lead to uncomfortable swelling, high blood pressure, and a lot of strain on your heart. If a fluid restriction becomes necessary, your doctor will give you a precise daily limit to follow. This limit includes everything that’s liquid at room temperature—think water, ice, soup, and even gelatin.
Are All Plant-Based Diets Good for Kidney Disease?
A healthy, whole-food, plant-based diet can bring some major benefits to kidney health, but the quality of that diet is everything. A plan centered on fresh fruits, vegetables, legumes, and kidney-friendly grains is a fantastic choice.
The trap is in the processed vegetarian and vegan products you see in stores. These convenience foods are often packed with sodium and phosphorus additives to make them taste better and last longer on the shelf, which makes them a poor choice for a renal diet. It’s so important to work with your healthcare team to make sure any plant-forward diet you adopt is thoughtfully planned to meet your unique nutritional needs while avoiding these hidden additives.
At Medilux Ayurveda USA, we blend ancient Ayurvedic wisdom with modern guidance to support your kidney health journey. Our personalized treatment plans, including diet and lifestyle counseling, are designed to help you manage CKD and improve your quality of life. Explore our approach to holistic kidney care at https://mediluxayurveda.com.
